All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know AML.
The aml Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the aml Hub cannot guarantee the accuracy of translated content. The aml and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The AML Hub is an independent medical education platform, sponsored by Daiichi Sankyo, Johnson & Johnson, Syndax, Thermo Fisher Scientific, Kura Oncology, AbbVie, and has been supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group.
The funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View AML content recommended for you
Long-term follow-up of the EORTC-GINEMA AML-10 trial
The phase III randomized European Organization for Research and Treatment of Cancer-Gruppo Italiano Malattie Ematologiche dell’ Adulto (EORTC-GIMEMA) AML-10 trial assessed the impact of the type of induction and stem cell transplantation in younger patients with acute myeloid leukemia (AML).1 The trial was amended to include a second randomization to compare autologous hematopoietic stem cell transplantation (auto-HSCT) with peripheral blood stem cells (APBSCT) and auto-HSCT with bone marrow (ABMT) in patients in first complete remission (CR) following intensive chemotherapy who did not have a human leukocyte antigen identical sibling donor available.2
Here, we summarize the long-term follow-up data from the second randomization of the EORTC-GIMEMA AML-10 trial published by Baron et al.2 in American Journal of Hematology.
Study design and patient population2
- 292 patients were randomized to receive either APBSCT (n = 146) or ABMT (n = 146).
- Among the patients randomized to receive APBSC, 104 received APBSCT, and 6 received ABMT.
- Of the patients randomized to ABMT, 71 received ABMT, 17 received APBSCT, and 22 received ABMT followed by APBSCT rescue.
- The median age was 44 years (range, 15–60 years), and patient characteristics were comparable between treatment groups.
- While 22.3% of patients were not assessable, 19.9%, 51.4%, and 6.5% of patients were classified as favorable, intermediate, and adverse risk, respectively, according to the UK Medical Research Council classification.
- Median follow-up was 15.7 years and 16.0 years for the APBSCT and ABMT groups, respectively.
Key findings2
- The 5-, 10-, and 15-year disease-free survival (p = 0.48), cumulative incidences of relapse (p = 0.45), and overall survival (p = 0.52) rates from the second randomization were similar between treatment groups (Figure 1).
Figure 1. A 5-, B 10-, and C 15-year DFS, CIR, and OS rates from the second randomization in the AML-10 trial*
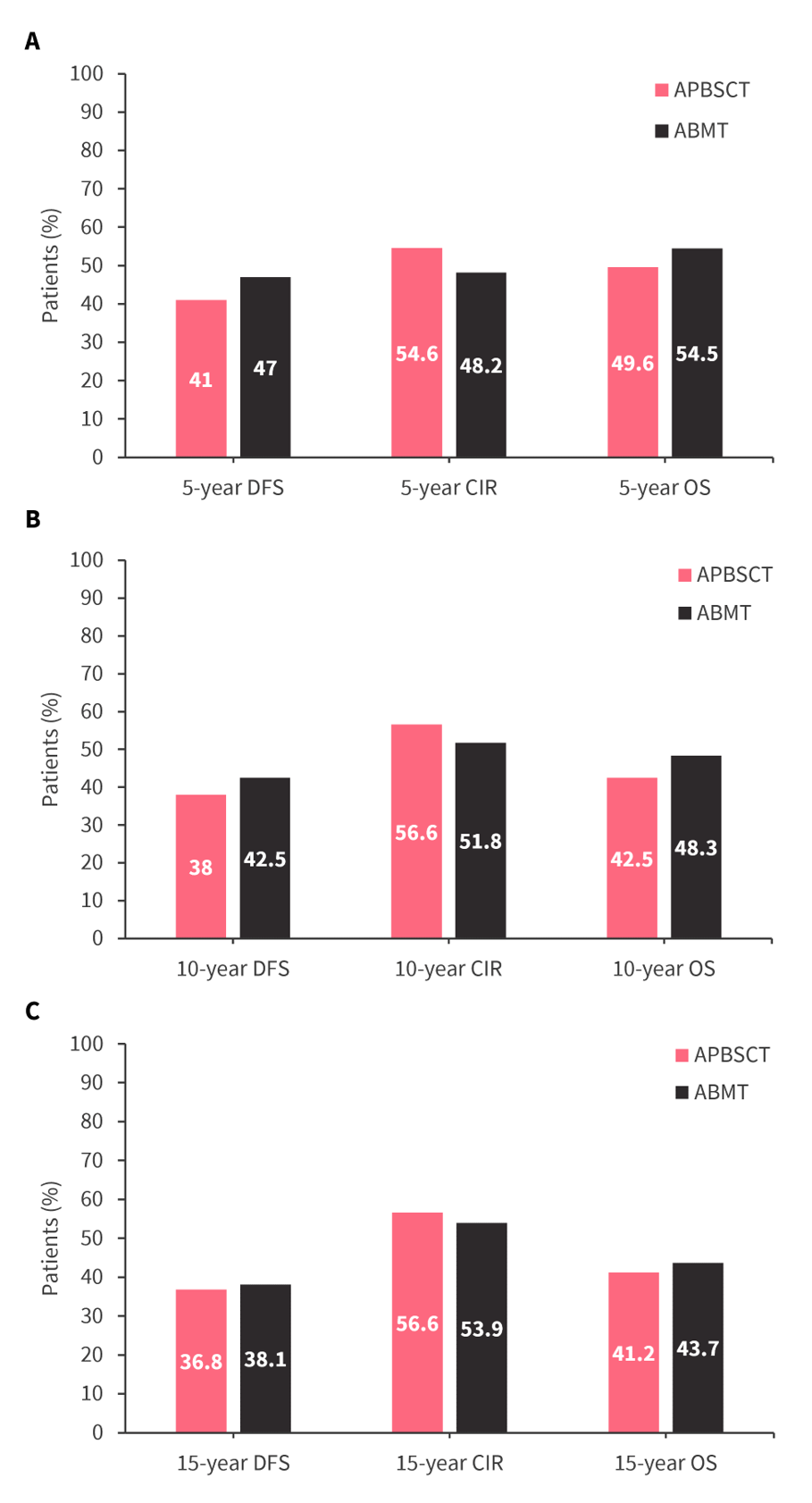
ABMT, autologous hematopoietic stem cell transplantation with bone marrow; APBSCT, autologous hematopoietic stem cell transplantation with peripheral blood stem cells; CIR, cumulative incidence of relapse; DFS, disease-free survival; OS, overall survival.
*Data from Baron, et al.2
- The 15-year disease-free survival, cumulative incidences of relapse, and overall survival rates among patients alive and still in first CR 5 years postrandomization were comparable between treatment arms Figure 2.
Figure 2. 15-year DFS, CIR, and OS rate among patients alive and still in first CR 5 years postrandomization in the AML-10 trial*
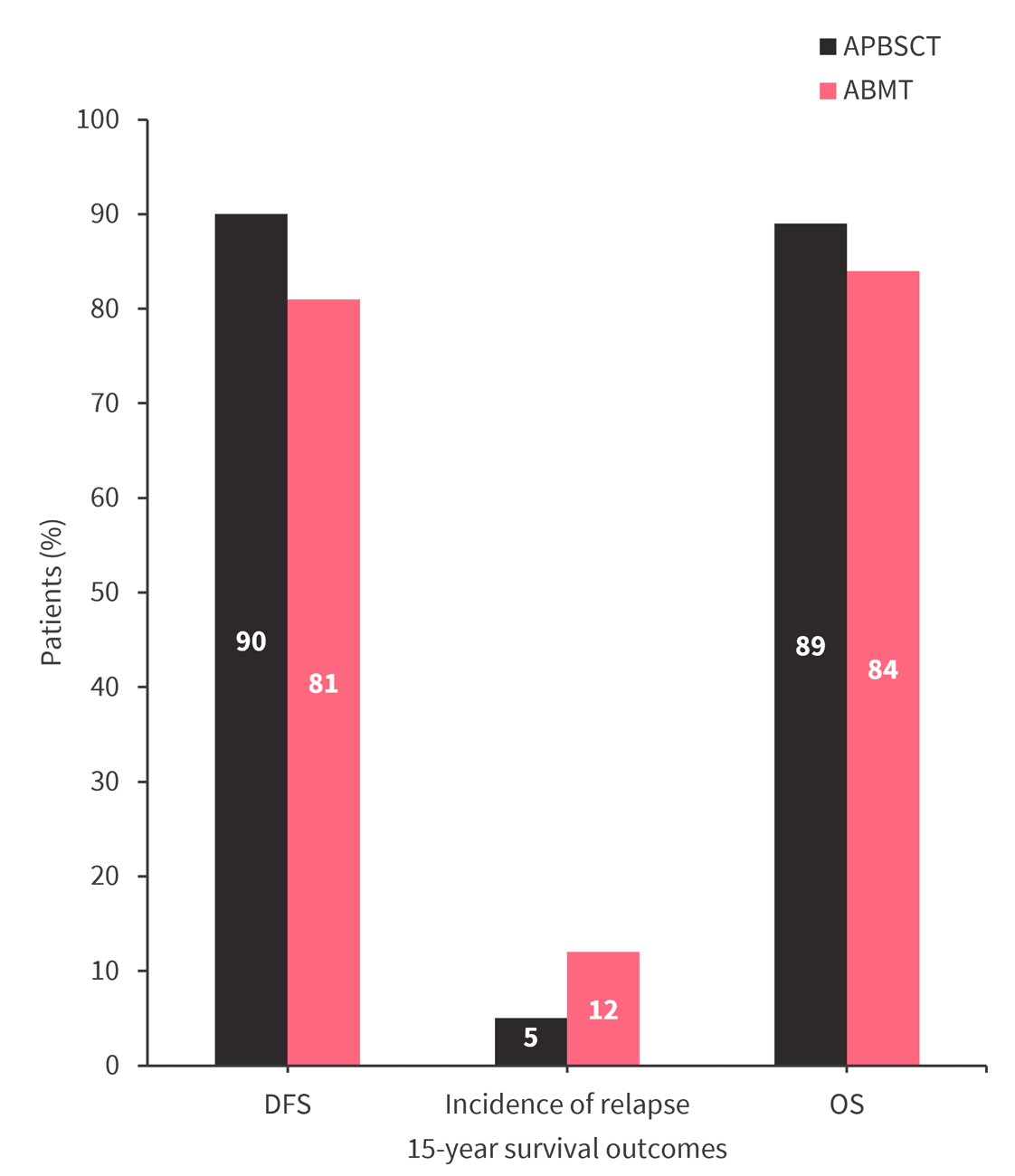
ABMT, autologous hematopoietic stem cell transplantation with bone marrow; APBSCT, autologous hematopoietic stem cell transplantation with peripheral blood stem cells; CIR, cumulative incidence of relapse; DFS, disease-free survival; OS, overall survival.
*Data from Baron, et al.2
- The 15-year cumulative incidence of death without relapse from randomization was 6.7% in the APBSCT group and 8.0% in the ABMT group.
- Multivariable analysis showed that cytogenetic adverse and intermediate risk, male sex, and higher CD43+ cell count (≥7×106 CD34+ cells/kg) in the apheresis product were associated with worse survival outcomes (Table 1).
Table 1. Multivariable analysis for DFS, CIR, and OS in the AML-10 trial*
|
CI, confidence interval; CIR, cumulative incidence of relapse; DFS, disease-free survival; H, highest count of CD34+ cells ×106/kg body weight during a single apheresis; HR, hazard ratio; MRC, Medical Research Council; OS, overall survival. |
||||||
|
Variable |
DFS |
CIR |
OS |
|||
|---|---|---|---|---|---|---|
|
HR (95% CI) |
p value |
HR (95% CI) |
p value |
HR (95% CI) |
p value |
|
|
MRC: Intermediate vs favorable |
2.69 (1.63–4.45) |
0.0001 |
2.63 (1.53–4.53) |
0.0005 |
2.66 (1.55–4.58) |
0.0004 |
|
MRC: Adverse vs favorable |
5.90 (2.94–11.80) |
<0.0001 |
7.02 (3.39–14.53) |
<0.0001 |
6.98 (3.37–14.5) |
<0.0001 |
|
Sex: male vs female |
1.41 (1.04–1.91) |
0.029 |
1.33 (0.96–1.85) |
0.085 |
1.36 (0.98–1.88) |
0.064 |
|
CD34 cell harvest: H ≥7 vs H <1 |
3.11 (1.64–5.87) |
0.0005 |
4.48 (2.10–9.54) |
0.0001 |
2.35 (1.24–4.44) |
0.0086 |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

